Americans grapple with chronic obesity, according to recent figures from the Centers for Disease Control and Prevention spanning from 1999–2000 to March 2020. The prevalence of obesity in the U.S. surged from 30.5% to 41.9% during this period, raising significant concerns given its association with Alzheimer’s, heart disease, stroke, type 2 diabetes, hypertension, and various cancers. In 2023 fiscal terms, the annual estimated medical costs linked to obesity in the United States neared $173 billion, making obesity-related health conditions the primary instigator of adverse health outcomes among Americans. Research also shows that obesity rates are often higher in low-income communities due to government subsidies of unhealthy food additives like high-fructose corn syrup and less access to nutrient-dense foods. A potential remedy for obesity could not only foster a healthier nation but also lead to a substantial reduction in healthcare expenditures and economic mobility for the truly disadvantaged.
That America has an obesity problem is no surprise. A wide variety of “solutions” are on offer from diet gurus, traditional healthcare practitioners, and social media fitness influencers. How can those in the church find the narrow gate of healthy living and avoid the wide road of bodily destruction—without judgment and shame?
Regarding obesity prevalence within the American Christian population, Christina Marini correctly identifies the crucial role played by the consumption of nutrient-deficient, high-calorie foods in substantial quantities, the intake of sugary beverages, and insufficient physical activity in contributing to obesity development. Yet, does the Christian lifestyle in America serve as a protective factor against these contributors? The data paints a disheartening picture. A study conducted by the National Institutes of Health, spearheaded by Matthew J. Feinstein, discovered that young adults who regularly participated in religious services were 50% more likely to experience obesity by middle age.
While Christians conscientiously address vices that undermine the stewardship of their bodies, churches often neglect the community norms that contribute to obesity. This prompts a crucial question: How should Christians respond to this phenomenon?
What Is Obesity? Where Does It Come From?
Paraphrasing the definition offered by the Obesity Medicine Association, obesity is a disease state resulting from maladaptive alterations in normal physiologic, biochemical, and neurohormonal function. In short, much as with diabetes, cardiovascular disease, and many other conditions, obesity is a chronic disease whose cause and progression lay somewhere in the intersection between abnormal unconscious processes and personal decisions. Interestingly, in obesity much of one’s volition is directly under the influence of self-propagating, abnormal biology. Unfortunately, rampant mischaracterization of this condition has led to a long history of inappropriate advice ranging from ineffectual to detrimental. If we are to see radically different results, we are going to need a radically different understanding in our approach to this devastating and costly epidemic.

Some generalities can be discussed as we consider the causes of obesity. On an individual basis, we now know this to be a very heterogenous disease with interplay to varying degrees between genetics, nutrition, sleep, hormones, environment, and, often, prescribed medications. Of these, all but genetics are modifiable factors. While all these factors need to be addressed, the area most ubiquitously discussed is nutrition—particularly as it relates to the “Western diet.” By this we are typically referring to the relatively inexpensive, ultra-processed, highly palatable, highly convenient, high glycemic index foods—think chips, fries, sodas, cookies, etc. Add to this the more natural starchy staples like potatoes, white rice, white breads, and cereals, and there is little wonder we are swimming in insulin resistance.
Is Obesity the Same as Gluttony?
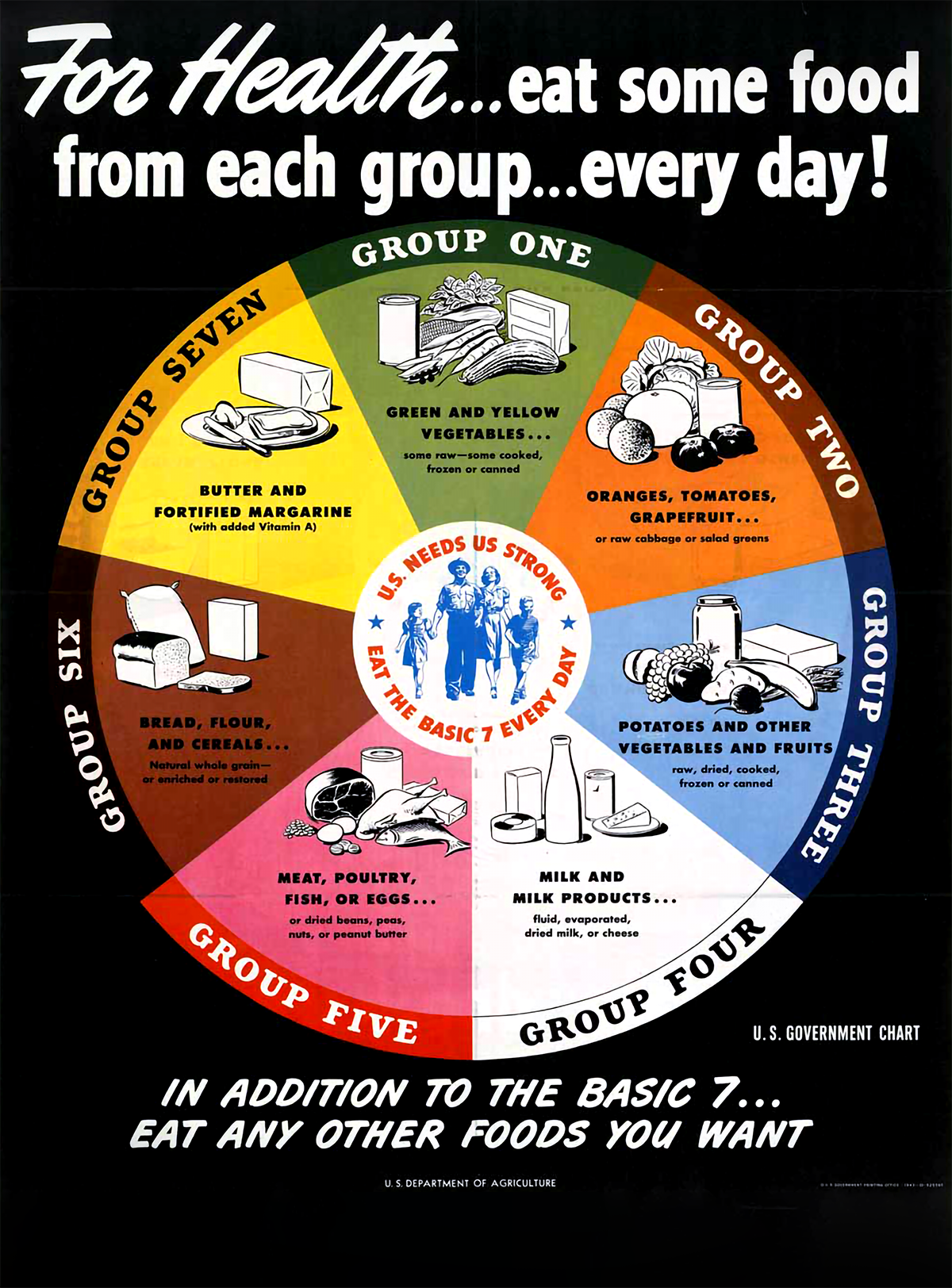
In ethical terms, it is essential to distinguish between obesity and gluttony. Western food production and processing methods often lead individuals to remain overweight despite adhering to the recommended dietary guidelines issued by the U.S. Department of Agriculture or those advised by numerous physicians. Even a diet that cut down on less-healthy foods might not guarantee the shedding of unwanted stored fat. Obesity frequently results from poor nutritional choices rather than mere overconsumption, setting it apart from the concept of gluttony.
Gluttony does not always manifest as obesity.
Thomas Aquinas, in Summa Theologica (2.2 Q. 148), clarifies that “gluttony denotes, not any desire of eating and drinking, but an inordinate desire.” The Christian scriptures explicitly condemn the inordinate desire for food and drink (Deut. 21:20; Prov. 23:1–3, 19–21, and 28:7). Notably, gluttony does not always manifest as obesity; factors like metabolism, food types, and other elements can prevent weight gain despite excessive food consumption. This implies that one can maintain a slender physique while displaying gluttonous behavior, even following a raw vegan or vegetarian lifestyle. Gluttony pivots more on the usage of food rather than solely correlating with obesity. Additionally, certain medications can induce weight gain, complicating the definition of obesity and necessitating a nuanced approach involving knowledge and empathy in addressing it.
Throughout the history of God’s people, overconsumption has always been denounced. Jesus faced allegations in the Gospels of being a drunkard and glutton (Matt. 11:19). Paul’s teachings to the churches highlight the perils faced by a community whose lifestyle revolves around their appetites, noting that “their god is their stomach” (Phil. 3:19). Complicating matters, excessive consumption often emerges as a coping mechanism for discomfort, pain, past trauma, or as a means to control a chaotic life. Early habituation of children to use overconsumption as a solution to emotional distress can pave the way for addiction. The act of eating triggers dopamine release in our brains, forging associations between pleasure centers and certain activities, whether virtuous or encouraged by vice. Research suggests a significant correlation between adult overeating and childhood trauma, revealing profound and intricate reasons behind a lack of self-control. Addressing these fundamental issues forms the cornerstone of a wise dietary approach in harmony with God’s intent for nutritional sustenance and enjoyment.
What Does the Bible Say About How Christians Should Eat?
While there exists a general consensus within the Christian tradition regarding God’s provision of food for humans to enjoy (Gen. 1:29), the production of food to satisfy their needs and fulfill the task of “ruling and subduing” the earth (Gen. 1:28), and the responsibility to “work and take care” of creation (Gen. 2:15) in order to cultivate food, significant disagreement arises concerning specific dietary practices. For example, Leviticus 11 outlines dietary laws categorizing animals as “clean” or “unclean.” Creatures with scales and fins (such as fish) and mammals possessing split hooves and that chew their cud (e.g., deer, cattle, goats) were deemed clean (Lev. 11:7–9), while crustaceans (like shrimp, lobsters), rabbits, pigs, and similar animals were considered unclean. These prohibitions aligned with the directive for God’s people to be “set apart” (Lev. 20:26) from the surrounding pagan nations that did not worship the one true God. Thus, they were instructed not to consume foods offered to idols but to recognize that food consumption held spiritual and sacramental significance. Their dietary practices aimed to demonstrate their distinctiveness to neighboring nations.
Paul’s teachings highlight the perils faced by a community whose lifestyle revolves around their appetites.
The resurrection of Christ nullified the use of these dietary restrictions that distinguished between Jews and Gentiles (Acts 10–11; 1 Tim. 4:4). The sanctification and distinction of God’s people now stem from their faith and trust in the work and person of Jesus Christ, not their dietary preferences. Jesus himself declared all foods clean (Mark 7:19), emphasizing the importance of the condition of one’s heart rather than the specific foods consumed in relation to union or disunion with the Triune God. In other words, holiness no longer hinges on adherence to the Old Testament dietary laws but rather on the spiritual nourishment of the heart in union with Christ, providing the freedom to exercise discernment and wisdom.
Christians across various traditions hold differing opinions on the persistence of Old Testament dietary restrictions, not in terms of holiness but regarding wise and healthy living. Some argue that the dietary laws outlined in the Bible also represent the healthiest dietary choices. Drawing from Genesis 1 and 2, certain individuals might advocate for vegetarianism, while others could support a more generalized pescatarian diet. Conversely, some might argue for the permissibility of all types of meat consumption. After the resurrection of Jesus Christ, the Bible underscores that dietary directives assume a secondary role. What is crucial now is the application of knowledge and prudence rather than strict adherence to dietary laws. Therefore, this article can only offer insights based on the best available information regarding our food options and their alignment with our bodily needs.
What’s a Wise Diet?
What constitutes the optimal diet for promoting good health? Is it keto, paleo, Mediterranean, or vegan? They all can have potential health benefits, particularly concerning weight loss among individuals with obesity. For many, the Mediterranean diet boasts the most compelling evidence, specifically with respect to cardiovascular advantages. All these dietary approaches possess the potential to enhance health; however, they can also be misused, resulting in adverse health effects. In the absence of more definitive research, I (Jones) have come to believe that amid these theories, the most beneficial nutritional guidance entails integrating these dietary plans into what I refer to as a C.L.E.A.N. dietary pattern.
C.L.E.A.N. signifies foods that are Clear of most, if not all, additives and preservatives, have a Low glycemic index, are Eclectic in variety, Anti-inflammatory, and Nonprocessed—as much as possible. In essence, these foods are composed of ingredients that are easily pronounced—such as fish, avocado, spinach, whole grains, etc. While not all processed foods need be off-limits, a diet primarily reliant on packaged foods likely forms an unsound dietary foundation. If you lack culinary skills, it is essential to learn some, as good health doesn’t come prepackaged. Additionally, water plays a crucial role in a healthy diet. If you are not naturally inclined toward drinking water, it is important to develop that habit. Considering that almost 80% of your body consists of water, embracing it is pivotal for good health. Transforming your perspective can be as simple as adding the word “yet” to your vocabulary, as in, “I do not like water, yet!”
The key to enhancing health, including reducing excess body fat, lies in improving the quality and chemistry of the fuel nourishing your organs. Anything consumed gets either absorbed into your bloodstream and distributed to every cell or eliminated as stool. As critical as food volume/caloric intake and exercise are, nothing surpasses the significance of ingesting fuel that enhances physiological function. It’s often said, “You cannot outrun a bad diet.” While one can be slim despite an unhealthy diet, there are countless unhealthy, slim individuals. If your aim is to shed weight and achieve sustainable good health, you must build a dietary foundation that supports normal organ function while minimizing dysfunction—the essence of the C.L.E.A.N. dietary pattern.
Knowing what to do is not sufficient, however. Merely possessing knowledge about healthier living usually results in, at best, temporary weight loss followed by regained pounds, and often additional weight gain. In reality, over half of those who lose weight regain most of it within four years or less, and up to 90% regain at least some weight without rigorous, long-term management. Frequently, our desires drive us toward detrimental behaviors while deterring us from beneficial ones. While our bodies benefit from certain practices, our desires lead us in conflicting directions. Since we cannot alter what is beneficial for us, our only recourse is to change our desires. Thankfully, although it demands time and effort, desires, habits, and patterns can be learned and cultivated. Rather than dedicating energy to shedding a few pounds, we should focus on adopting healthier habits with the ultimate goal of transforming our desires. Obesity is not fundamentally a weight problem; it’s a want problem—we possess a “broken wanter.”

Cultivating changes in our habits, routines, and even desires may begin by rectifying our lack of knowledge concerning healthier living, but this alone will not suffice. Repeatedly integrating these practices into our daily routines should aim not merely at dropping some weight but gradually normalizing these healthier behaviors, eventually making them desirable. Falling in love with the process leads to lasting results; loving the end results often yields fleeting outcomes. Indeed, the ongoing treatment for obesity resembles the gradual, methodical learning process of mastering a musical instrument more than the traditional approach to curing a disease.
I Am Overweight—What Should I Do?
What are some things we can begin doing today to stop “throwing gas on the fire” of this disease? Even though the calories-in, calories-out (CICO) model and lack of exercise are not the causes of the underlying pathophysiology of the disease of obesity, these are the most readily available points at which we can avoid fanning the flames and even help douse the fire. The following recommendations do not consider portion sizes, specific macronutrient proportions, or caloric intake, as these need to be individualized based on health goals, current health concerns, and individual preferences. Of course, it is also important to avoid even the recommended foods in cases of intolerance, allergy, or specific instructions from your healthcare provider.

We can start with a few nutrition recommendations. First, and perhaps most important, is eliminating or at least avoiding ultra-processed foods as much as possible. These are industrially manufactured food products that contain considerable amounts of additives and are often high in sugar, potentially less healthy fats, and salt. Mounting evidence suggests the detrimental effects of these types of foods comes largely from significant increases in the glycemic index (degree and speed with which a food causes spikes in blood sugar and insulin levels) and promotion of inflammation—your body’s immune response, which when overexcited can damage the body—resulting from the processing as compared to the same foods in their whole, natural state.
Other foods known to have inflammatory effects include processed and refined carbohydrates such as white bread, pasta, and sugar. Foods such as french fries and fried chicken are often fried in less healthy oils that can be pro-inflammatory. Processed meat such as bacon, sausage, and hot dogs have additives and preservatives that can cause inflammation. High-fructose corn syrup found in many processed foods and sweetened beverages can also promote inflammation; there is even convincing evidence for its role in the development of fatty liver disease that can progress to fibrosis, cirrhosis, and even cancer. Dairy products can trigger inflammation in some people, especially those who are lactose intolerant or have a dairy sensitivity. Alcohol can increase inflammation in the body, especially when consumed in excess. Vegetable oils (seed oils) such as corn oil, soybean oil, and safflower oil have high levels of omega-6 fatty acids, which can promote inflammation if consumed in excess.
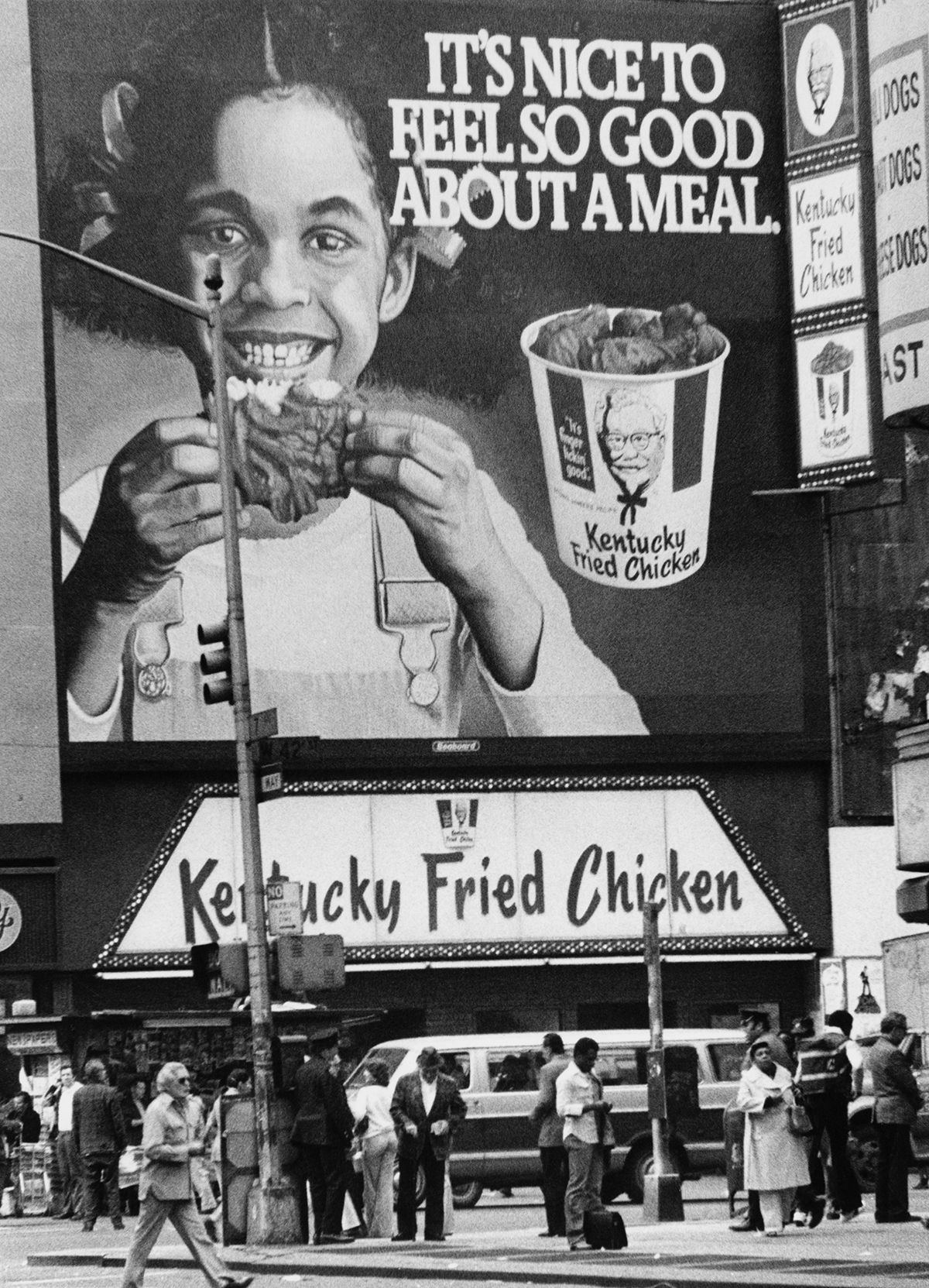
Unfortunately, many of the foods in the preceding two categories have become exceedingly difficult to eliminate, as over the past four to five decades they have become foundational to the Western diet.
All this raises the question, “What should we be eating?” Some important types of foods to consider—remember, tastes are learned and based largely on repeated exposure—are those with a low glycemic index that are high in fiber, high in protein (particularly those high in the essential amino acid leucine in its natural form, not supplemented by a capsule), higher in heart healthy fats, and preferably with anti-inflammatory properties, or at least those to which inflammation has not been attributed. Finding foods that meet all these criteria can be a bit challenging, but here are some options that come close: chia seeds, lentils, salmon, and almonds. (A quick Google search can give you more options.)

Now that we have some idea of both ends of the healthy vs. less healthy food spectrum, what are some foods that fall more in the middle that we will need in a healthy diet for improved variety as well as necessary nutrients perhaps not found in the preceding list? The following recommendations focus on different nutritional characteristics. You will notice that there is significant overlap among these lists, as some of the healthiest foods are considered healthy precisely because they contain elements of a variety of desirable characteristics.
Here are some low glycemic index foods that are known to have anti-inflammatory properties or are noninflammatory and should be at the top of your list: leafy greens, fatty fish, nuts, berries, turmeric, ginger, and green tea. High-fiber, low glycemic index foods are great choices for supporting stable blood sugar levels and promoting overall health. Examples include some legumes, vegetables, fruits, whole grains, nuts, and avocado.

The importance of exercise for health improvement and maintenance is vital. For many with obesity, however, some exercise recommendations range from lofty to downright undoable. It is important to note that these are goals to be worked toward. We should not take from this that anything less is worthless. It used to be said by many healthcare professionals that if you were not breathing hard and sweating you were not doing any good. More recent evidence from clinical trials and retrospective analyses has convinced most of us working in this space that this notion is utter bunk. While achieving the activity targets is recommended, any movement over nonmovement is good. Any movement—housework, yard work, gardening, cooking, rolling on the floor with the dog, standing when you could be sitting—is beneficial and preferable to being sedentary.
Finally, we should also briefly consider what are known as anti-obesity medications. There are several used under this heading, but most notable of late are the injectable therapies. Ozempic has been the most widely discussed by various media; however, it is actually a brand specifically indicated for use in diabetes. At this time, those approved for obesity include Saxenda, Wegovy, and the most recently released, Zepbound. Utilized properly, these can be a very beneficial part of a comprehensive obesity treatment plan. Despite much negative press, the risk of their use in the right patient population is fairly minimal and greatly exceeded by their benefits. It should be noted that they should not be used by those who are not obese but who would simply like to “lose a few pounds.”
Paul’s teachings highlight the perils faced by a community whose lifestyle revolves around their appetites.
One may reasonably ask, why would we consider the use of medication at all if radical, long-term lifestyle modification is the key to successful treatment? The answer is twofold. First, as previously established, there are physiological abnormalities present in obesity that, for many, no amount of good nutrition or exercise will overcome. Second, the tools used in obesity, including medications, in my opinion, should not be used for “weight loss” per se. Rather, they should be used in support of the needed changes. Consider the use of a jack to change a car’s flat tire. The person who desires to get the tire changed cannot do so with out jacking up the car. But the jack cannot change the tire. Anti-obesity medications are simply part of the “jack” that can be used to bear some of the burden so the needed lifestyle changes can be undertaken, but ultimately the burden of the changes still lays with the individual.
How Can Churches Encourage Healthy Living?
In 1 Corinthians 6:12, Paul writes, “All things are lawful for me, but not all things are helpful. All things are lawful for me, but I will not be dominated by anything.” While our church community should strive to promote “love and good works” (Heb. 10:24), we must also exercise caution not to lead our fellow believers into perilous situations needlessly (cf. Rom. 14:20, 1 Cor. 8:9). While spiritual well-being holds ultimate importance for the redeemed, Paul nevertheless instructs Timothy that there is “some value” in attending to the physical body (1 Tim. 4:8). It appears that the church generally heeds Paul’s advice concerning spiritual health; however, we often overlook our responsibilities concerning the physical well-being of our fellow believers’ earthly temples (cf. 1 Cor. 3:16, 2 Cor. 5:1).
We must confront the prevalent culture of church fellowship and communal meals.
Members of the body of Christ, although set apart, remain influenced by our culture. Addressing the obesity epidemic on a grand scale will necessitate reeducating and transforming our cultural norms regarding its causes and remedies. Yet, within the church, the goal might be more achievable. Contrary to some suggestions, we disagree that obesity is primarily a spiritual issue. Nonetheless, we do believe it holds spiritual implications to varying degrees in different individuals, whether as a causative factor or in its effects. We are not implying that all individuals grappling with obesity in the church struggle with gluttony, but some might. Perhaps a fair assessment could refer to Paul’s assertion in 1 Corinthians 6:12 regarding being “dominated.” Are you controlled by food in general or specific types of food? Remember, it is not merely about enjoying a particular food but whether that food exerts control over you. Where the issue carries spiritual weight, be it causative or consequential, compassion, understanding, accountability, repentance, restoration, and, significantly, acknowledgment of forgiveness through divinely appointed means of grace should be extended, as with any other spiritual struggle, rather than dismissing it as insignificant.
Moreover, practical steps must be considered to engage with the issue of obesity within our church community. Here are a few initial suggestions. First, rather than ignoring obesity, we must be willing to gently acknowledge its existence. Only then can we identify the church’s role in propagating and even enabling the problem. This acknowledgment paves the way for considering how we can aid those in need within our congregations.

Additionally, we must confront the prevalent culture of church fellowship and communal meals. Reflect on the various food lists mentioned earlier. If you examine the typical offerings at a church social event and compare them to these lists, would you assume that those partaking are more likely to be healthy or unhealthy individuals? You might argue, “We don’t eat like this all the time.” On average, however, the reality suggests otherwise. Why? Primarily, because we inhabit the same culture where unhealthy eating is commonplace. Simply claiming that many of those consuming the same food are not overweight is not proof of their good health. Rather than most of our non–Sunday service activities being largely sedentary, to help reduce our food focus perhaps we should consider types of gatherings that promote movement, from church-wide social and ministry gatherings to community-service projects.
Conclusion
The act of sharing and savoring food represents a beautiful, divine blessing. But our reality is fraught with the complexities of modernized food production, conflicting dietary information, and shifts in traditional eating habits. It’s an overwhelming web of confusion—today’s dietary villain was yesterday’s health hero. Frustration is inevitable. However, as a community bonded by faith, we cannot endorse excessive consumption or unwise eating. We grapple with the solution, but acknowledging obesity as a critical concern is our first step. Normalizing healthier communal living and supporting those battling obesity within our midst is essential. Let’s shift our focus during gatherings away from unwise eating habits and toward healthier options without stigma or judgment. Encouraging gratitude for those who provide these choices is a start. Addressing obesity not only improves our health but also diminishes healthcare costs and enhances economic opportunities for the most vulnerable among us. This journey toward healthier living is one we must embark upon together, shaping a brighter, more nourished future for all.









